Wow. I thought I knew almost everything about open-heart surgery and post-operative care but I was sorely wrong. Nothing prepares you for being a spouse or primary caregiver for a loved one after  open-heart surgery. I’m talking about the care you provide at home after receiving a “zipper” – the common term for full sternal or partial sternal surgical entry to the heart. I have worked in open-heart recovery in a large medical center, ICU, and cardiac and pulmonary rehabilitation, but I was not completely prepared for home recovery.
open-heart surgery. I’m talking about the care you provide at home after receiving a “zipper” – the common term for full sternal or partial sternal surgical entry to the heart. I have worked in open-heart recovery in a large medical center, ICU, and cardiac and pulmonary rehabilitation, but I was not completely prepared for home recovery.
Our Story
My husband had significant mitral valve regurgitation for four years. We knew a valve repair or replacement would be in our future. We also knew we would be in a position to schedule the surgery as the condition worsened, unless of course, something urgent happened, such as a rupture of his mitral valve chords or similar. With that said, we were able to schedule the surgery and thought we were well-prepared for the post-operative care at home.
The surgery overall went well and the care was outstanding by the cardiac care unit nurses. We received lots of discharge education which, especially if you are tired, becomes a blur after a while. The new concept is patient-centered care so, with the education component of care, the education is directed toward the patient. Looks can be deceiving. A patient may look alert and oriented times three (know his/her name, date, location, and name of the president) but it doesn’t necessarily mean they can remember all the education and tips that are shared by occupational therapy, physical therapy, social work, and the Phase I cardiac rehab nurse. I attended all the bedside teaching I could so we could be prepared. But even with my healthcare background, my eyes were opened to some new things to consider as a spouse or caregiver.
Tips for After Open-Heart Surgery
There is a lot that goes on during those three to four weeks at home before someone heads off to cardiac rehab. Depending on the condition, the doctor(s) could be controlling the heart rhythm, managing fluid retention, or helping a patient manage pain. The overall plan is generally to stabilize the patient and get them ready for cardiac rehab as soon as possible.
13 Tips to Help Care for Your Loved One:
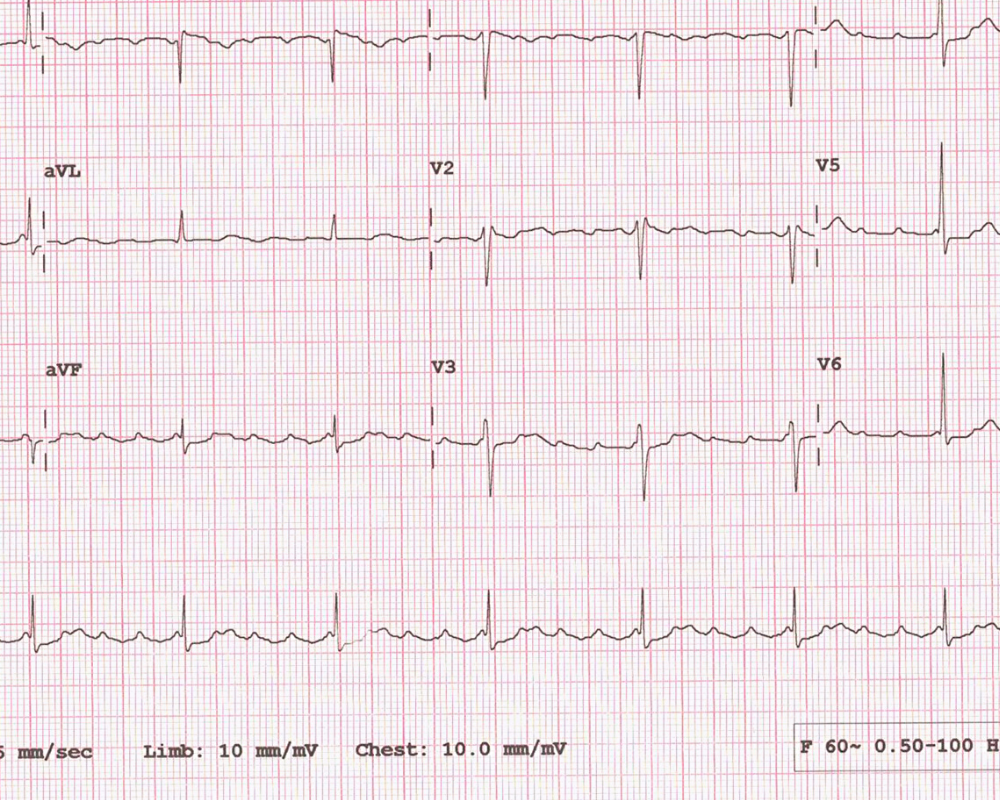
- Get your supplies in order before discharge. At a minimum, have a precise weight scale, blood pressure cuff, thermometer, shower chair or similar (we used a small, short ladder that had a seat on it), bandaids, over the counter steroid cream for skin irritations from a variety of sources, and anti-bacterial soap. “Nice to haves” would be a pulse oximeter and the new two-lead EKG monitors that are available on the market now. A tape measure or stick is helpful to measure things like the sternal or chest tube incision sites.
- Your loved one may not be able to sleep in the bed for four to six weeks. I should have picked up on that considering we were discharged and my husband was sleeping at a 90-degree angle in the bed in the hospital and we could not lower his head. I reviewed lots of literature online and received anecdotal information from friends who had valve repairs and bypasses. A common theme was, “Oh yeah, I couldn’t sleep in the bed for two months. I slept on a couch upright in the basement.” Apparently, this is more common, but then my dad had open-heart surgery with multiple complications and slept in a recliner for most of the last 10 years of his life. We received an excellent lecture on redeveloping good sleep habits after surgery but somehow, we both missed the “and don’t be surprised if you can’t sleep in the bed for a good long while.” Fortunately, my husband’s cardiologist and pulmonologist recognized my husband still had a 1/2 liter of fluid in each lung, and after three heavy days of diuretics, he was able to start sleeping in the bed – after four weeks of a recliner!
- Your life will turn upside down for at least four weeks. If your spouse or loved one is having to sleep in a recliner, that is a life-changer in itself. He/she will not be able to lift more than 5 lbs and will have restrictions with bending and turning. You may be managing the household all by yourself and suddenly you realize that the 15 minutes that are given by the other party to load the dishwasher and wipe down countertops become very valuable. He/she may need help even with bathing, dressing, and definitely with putting on TED hose. This leads me to #4.
- Learn how to put on TED hose. I knew how to put on TED hose from my years at the clinical bedside TED hose application has not changed. I wish it had but it hasn’t. Don’t leave the hospital without instruction so you don’t get frustrated at home. Plastic kitchen gloves do help with getting traction with the hands.
- Say Yes to Help. If your friends say they want to bring over dinners, let them. I honestly thought I could do it all but there was nothing so wonderful as to receive a main dish, soup, salad fixin’s, a nice dessert treat, or even a bit of bread. You will be doing a lot and no matter how much you have stored in the freezer, a homecooked meal beats take-out any day of the week. Just let your friends know you to watch the added salt and, if your loved one is on a blood thinner, share with them tips about managing foods high in Vitamin K.
- Smile at your new medical gear – your dining room table will make you feel old! The dining room table tends to be the dumping ground for multiple meds and healthcare devices. If you are new to managing illness with lots of medications, you will get a good laugh and a self-awareness moment that aging has arrived.
- Celebrate the small wins. Keep a log. Wins may include daily weight loss (that is anticipated and wanted), taking a bath independently, and buckling pants after water weight loss. Your loved one may also be thrilled when the appetite returns, he/she can drive, shortness of breath or pain is improved and wounds start to heal.
- Know what normal and abnormal look like. Be prepared to inspect your loved one daily. My husband had an allergic reaction to iron supplements. He broke out in a terrible rash, and although not particularly itchy, the inflammation spread around his incision site. After a process of elimination, we determined with the doctor it was the iron tablets. Once he stopped taking them, it resolved over four to five days. Track all concerns and progress on paper. Portable devices are great to track some things but you need to be able to see your log while you talk to the doctor, nurse, home care staff, etc.
- Be prepared for a lot of follow-up doctor visits. It is what it is. At a minimum, your loved one may be going to a coagulation clinic for INR readings and blood thinner adjustments. This is extraordinarily important to prevent the possibility of blood clots forming. Be prepared with questions, report progress with details you have gathered at home, and pushing your concerns if necessary.
- Ask for a home health nurse if you are not offered one. We were offered a home health nurse for the first two weeks. This was a Godsend as the nurse was able to draw the INR and other lab work during those two weeks of adjustment at home. She listened to his lungs for congestive heart failure, evaluated the incision, and reported to the doctor. She was a great point of contact with the doctor. In some cases, depending on the agency’s connections to the health system, the home health nurse may also have some access to your health record thereby improving the flow of communication.
- Vital signs and assessments will consume you. Create your own log to document everything from vital signs, incentive spirometry readings, cough production, temperature, and weight to activity level and medication changes, and quality of life. It is also nice to track other activities of daily living changes such as the day your loved one can sleep flat or put on socks. Many electronic health record systems have a patient healthcare tracking tool that the provider can activate and allow the patient to input specific data into the electronic file. I personally like to write things down to see improvements but that is just me.
- Be prepared for some isolation. It’s not uncommon for patients to experience depression after open-heart surgery. Feeling depressed and isolated is a BIG deal and I won’t go into detail of what I know about how the chest wall is manipulated during surgery, the tools used, etc. I get creeped out just thinking about it again as I write these thoughts. What is most important is to be kind and patient with your loved one. He/she may not feel like talking on the phone because of a raspy throat or a lingering cough. Stay in tune with what you observe, and if you have concerns, report them to the doctor.
- TCOY. Take care of yourself. Sounds easier than it is, but it is important to do something for yourself that is important to your well-being. For some, it is exercising once a day. For others, it may be journaling, cooking a small meal for enjoyment, taking a nap, or just being with a friend. Determine what are two to three things that are really important to your well-being and incorporate them into your week. Notice I did not say “day” because I have learned every day during the first month is an adventure. There is a medication change here, and an X-ray there. Go with the flow and figure out what works for you. Now is not the time to be a martyr. Your loved one needs all of you.
- BONUS! Enroll and attend in a cardiac rehabilitation program. These programs include not only exercise but helpful education programs such as nutrition and stress management that are excellent for both the patient and spouse!
Every patient post-opened heart surgery responds differently during the home recovery stage. At best, things go smoothly, medication adjustments are minimal, the appetite comes back, activity tolerance increases, and socialization returns as well. Yes, there are norms, but it’s important for caregivers to be as prepared as possible for the initial recovery process at home.
Happy healing!
Want More Plant-based Recipes, Videos and Tips?
ALSO AVAILABLE ON MY AUTHOR PAGE ON AMAZON!
CLICK ON THE IMAGES TO WORKBOOKS and COOKBOOKS








Thank you for sharing such a nice and informative Blog.
Early Signs Of Diabetes
Thank you! I hope it helps someone! Have a great day!
You are most welcome!